Must Reads
The proper functioning of the vagus nerve is vital to both physical and mental well being.
That post-prandial fatigue you get after eating a large meal? You can chalk that up to the vagus nerve (in part).
The vagus nerve provides a bidirectional link between gut and brain and connects all major organs (excluding the thyroid and adrenal glands). Believe it or not, the vagus nerve even plays a role in neurogenesis or the birth of new neurons. Gebhardt N. et al.9 showed that vagus nerve stimulation promotes neurogenesis in the dentate gyrus of animals after 48 hours of treatment.
In this article, I'll discuss common vagus nerve symptoms. These symptoms of vagus nerve dysfunction manifest when the vagus nerve is either hyper or hypoactive.
Hyperarousal
If you suffer from any disease that involves hyperarousal - like anxiety4, panic disorder, epilepsy, PTSD or insomnia - the vagus nerve likely plays a role.
The vagus nerve is also implicated in tinnitus (ringing or buzzing in the ears). Vagal nerve stimulation has shown promise as a treatment for tinnitus 3. Given that the vagus nerve regulates the gut, it is less remarkable that it plays a role in irritable bowel syndrome (IBS).
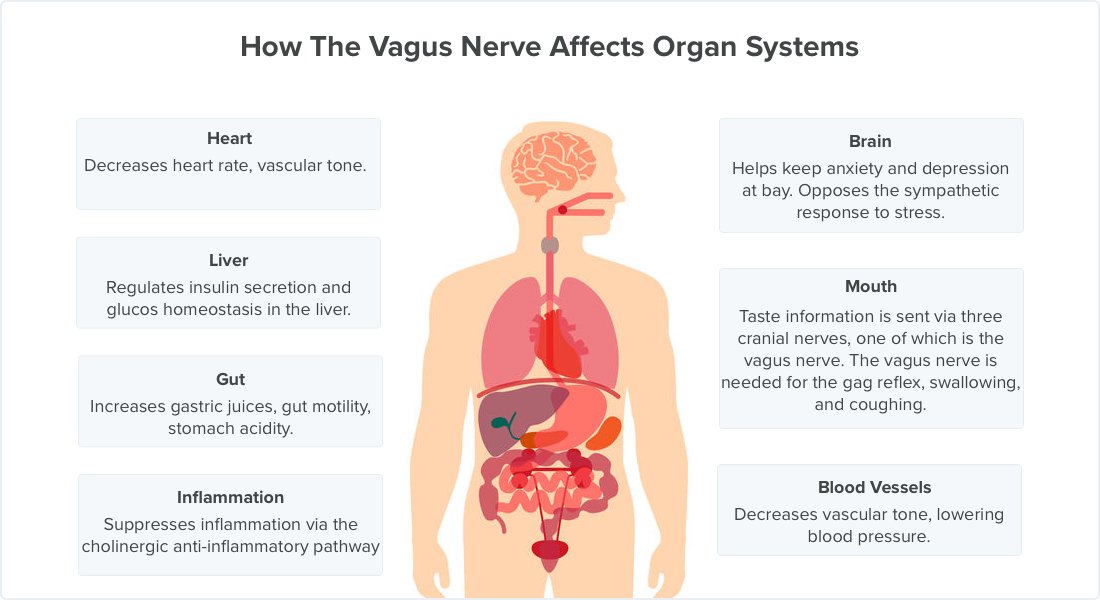
Vagus nerve activity promotes relaxation, lowers heart rate, and helps keep anxiety and depression at bay. Conversely, impaired vagus nerve function increases heart rate, blood pressure, the stress response and impedes digestion.
What Is The Vagus Nerve?
The vagus nerve is the longest cranial nerve in the body. It not only regulates the gut but also affects the cardiovascular, respiratory, immune, and endocrine systems. The vagus nerve innervates the liver, lung, spleen, kidneys and gut.
Here are some quick facts:
- Vagus is latin for wandering because the nerve has a long and circuitous path in the body
- Increased vagal tone is associated with increased intimacy and social boding. Conversely, isolation diminishes vagal tone1
- Vagus nerve activity has an antidepressant effect. The hypothalamic-pituitary-adrenal (HPA) axis stress system is out of whack in depression and vagal nerve stimulation normalizes dysregulation of the HPA axis 2.
- Vagus nerve dysfunction causes gastrointestinal symptoms. The vagus nerve increases stomach acidity, gut motility and digestive juices. A hypoactive vagus nerve results in delayed gastric emptying.
- The vagus nerve keeps inflammation in check. When the vagus nerve senses inflammatory cytokines it alerts the brain to suppress inflammation via the cholinergic anti-inflammatory pathway.
- Vagus nerve stimulation inhibits the synthesis of tumor necrosis factor (TNF) in liver, spleen and heart. Conversely removal of part of the vagus nerve (vagotomy) exacerbates TNF responses to inflammatory stimuli.
- Enterotoxin is responsible for the symptoms of food poisoning. Enterotoxin stimulates the vagus nerve and the vomiting center of the brain, resulting in sickness behavior.
Underactive vs Overactive Vagus Nerve
Both overactive and underactive vagus nerve activity can contribute to disease and cause vagus nerve symptoms.
For example, an underactive vagus nerve can lead to gasteroparesis or delayed gastric emptying. Normally, peristalsis - a rhythmic contraction and relaxation of the intestinal muscles pushes food into the small intestine for additional digestion. These contractions are under the control of the vagus nerve; damage to the vagus nerve impairs peristalsis.
An overactive vagus nerve can result in an abnormally low heart rate (bradycardia), fainting (syncope), and a range of other symptoms.
The Parasympathetic Nervous System
The vagus nerve interfaces with the parasympathetic nervous system. Vagus nerve activity regulates:
- heart rate (decrease)
- gastrointestinal peristalsis (increase)
- sweating (decrease)
- satiety from food (increase)
- inflammation (decrease)
- neural processes (decrease)
- neurogenesis (increase)
- glucose homeostasis and insulin secretion
The vagus nerve helps counterbalance the sympathetic innervation of the heart. The sympathetic arm of the nervous system is what mediates the fight-or-flight response.

Stressful situations - like taking an exam - trigger the sympathetic, fight-or-flight response.
The sympathetic response increases heart rate, anxiety, concentration, blood pressure, and sweating. Animals evolved this response to better help them cope with stress.
This sympathetic response is opposed by the vagus nerve. So you won't be surprised that the vagus nerve decreases heart rate and promotes rest and digestion.
Vasovagal syncope can occur with excessive activation of the vagus nerve due to a traumatic experience. Too much vagus nerve activity can cause a drop in cardiac output, resulting insufficient blood flow to the brain (cerebral hypoperfusion).
Symptoms of Vagus Nerve Dysfunction
The symptoms of vagus nerve dysfunction vary depending on whether the vagus nerve is overactive or underactive.
One of the most common symptoms of vagus nerve dysfunction is pain. Pain is often accompanied by muscle cramps on moving. This pain can be so severe as to interfere with walking.
Dysfunction of the vagus nerve can also cause difficulty swallowing. You may also lack a normal gag reflex if your vagus nerve is damaged. Since the vagus nerve controls some muscles in the throat, damage to the vagus nerve can also alter your voice.
Here are some common symptoms of vagus nerve dysfunction.
1. Obesity and Weight Gain
A few studies have linked decreased vagus nerve activity to obesity678. This makes intuitive sense given that the vagus nerve regulates insulin secretion and glucose homeostasis.
The vagus nerve plays a role in the satiety from food. Since vagal afferents transmit satiety signals from the gut to the brain. Hence, the vagus nerve would seem important for keeping appetite under control and helping to prevent development of obesity.
However, the picture is muddied by the fact that removal of the vagus nerve (vagotomy) does not cause excess eating or obesity. Moreover, electrical stimulation of vagal afferents does not appear to decrease food intake and body weight.
2. Irritable Bowel Syndrome (IBS)
Dysregulation of the autonomic nervous system plays a role in the development of irritable bowel syndrome (IBS).
Spaziani R et. al characterized the autonomic response to rectal distention in healthy volunteers and patients with IBS. Systolic blood pressure increased in response to rectal distension in all participants, but the increase was greater in patients with IBS. IBS patients also had lower baroreceptor sensitivity at rest and throughout rectal distention compared to healthy volunteers.
Greater systolic blood pressure response to rectal distension and associated diminished BRS suggests a compromise of the autonomic nervous system in IBS patients.
3. Depression
Vagus nerve dysfunction disrupts mood and can contribute to depression.
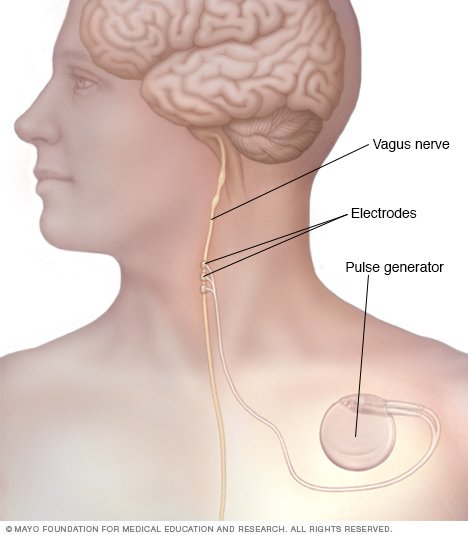
Vagus nerve stimulation has been used clinically since 1985, when Zabara et al. showed that electrical stimulation from the vagus nerve inhibited neural activity and suppressed seizures in dogs.
Currently, vagus nerve stimulation is an FDA-approved therapy for treatment-resistant depression.
Vagus nerve stimulation is often invasive (though less invasive methods are now available). Therefore, vagus nerve stimulation has historically been reserved for the most severely depressed patients.
The vagus nerve, which innervates the upper gut and proximal colon, has been implicated in anxiety and depression. Ingestion of Lactobacillus rhamnosus induced changes in expression of the inhibitory neurotransmitter GABA1b in neurons, associated with reduced levels of corticosteroids and reduced anxious and depressive behaviors. Remarkably, these changes could be blocked by vagotomy.
4. Anxiety
The connection between anxiety and the vagus nerve is well-known.
When functioning properly, the vagus nerve opposes the sympathetic, fight-or-flight response. Vagus nerve dysfunction leaves the sympathetic response unopposed leading to hyperarousal, anxiety, insomnia, increased heart rate and decreased rest.
Normal vagus nerve activity is needed to keep the fight-or-flight response in check.
5. Bradycardia (Abnormally Slow Heart Rate)
Bradycardia is a symptom of too much vagal activity. Technically, bradycardia is defined as a heart rate below 60 beats per minute. But marathon runner's have low heart rates due to an adaptive increase in cardiovascular fitness.
Decreased heart rate can lead to syncope or the temporary loss of consciousness. Bradycardia causes inadequate cardiac output, and poor brain perfusion, leading a syncopal episode (fainting).
An abnormally slow heart rate decreases cardiac output. Some runners with slow heart rates may be self-medicating by running to increase their heart rate.
6. Difficulty Swallowing
The primary motor division of the vagus nerve is the recurrent laryngeal nerve.
The recurrent laryngeal nerve is important for producing vocal cord adduction during bolus (food) passage and makes possible glottic closuring during the cough reflex.
Injury to the recurrent nerve leads to vocal cord paralysis. Symptoms include:
- dysphagia - difficulty or discomfort swallowing
- weak voice
- poor cough
Vagal nerve injury at or near the skull base causes pharyngeal motor weakness and a laryngopharyngeal sensory deficit which adds to the risk of aspiration.
Aspiration is the entry of material from the oropharynx or gastrointestinal tract into the voice box and lower respiratory tract.
7. Delayed Gastric Emptying
Gasteroparesis, also known as delayed gastric emptying, can be caused by a damaged or underactive vagus nerve. The vagus nerve helps coordinate peristalsis. Peristalsis is the contraction and relaxation of the muscles of the intestine, which creates wavelike movements that push food forward.
The symptoms of delayed gastric emptying include:
- nausea
- heartburn
- stomach pains
- spasms in the stomach
- weight loss
8. Vasovagal syncope

Syncope is the spontaneous and self-limited loss of consciousness. It's followed by prompt and complete recovery. The key feature of syncope is global cerebral hypoperfusion (insufficient blood flow to the brain).
The cause of vasovagal syncope is characterized by a reflex activation triggering a rapid decrease in heart rate and reduction in vascular tone 5. In the first moments of a vasovagal syncope an empty heart is seen via echocardiography because of the loss of preload (‘empty heart’ syndrome).
9. B12 Deficiency
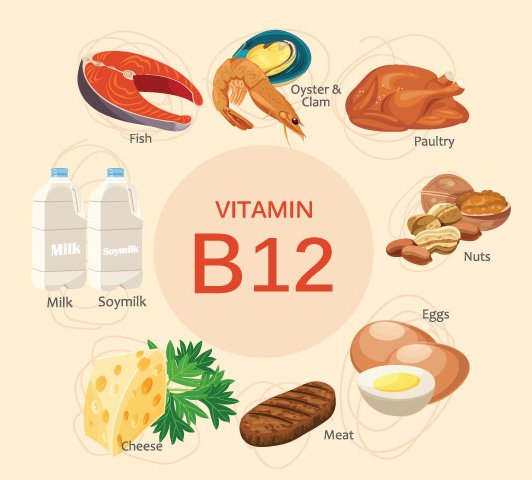
A serious side effect of vagotomy (surgical removal of part of the vagus nerve) is vitamin B12 deficiency. Why is this the case?
The vagus nerve normally stimulates parietal cells in the stomach to secrete acid and intrinsic factor. Intrinsic factor is needed to absorb vitamin B12. Vagotomy reduces intrinsic factor secretion, which impairs vitamin B12 absorption. Vitamin B12 deficiency - if untreated - results in nerve damage, dementia, and death.
10. Chronic Inflammation
"Chronic inflammation" is a nebulous term that's frequently misused by snake oil salesmen. Despite this unsavory association, no article on the vagus nerve would be complete mention without mention of inflammation.
In the young and healthy, inflammation is a local event that resolves on its own. But the innate immune response can be come disrupted resulting in continual pro-inflammatory cytokine activity. This state of chronic inflammations underpins a wide range of disease states, including sepsis, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, and possibly even Alzheimer's disease.
The Cholinergic Anti-Inflammatory Pathway
The inflammatory reflex is a mechanism under the control of the vagus nerve.
Parasympathetic outflows from the vagus nerve inhibit macrophage activation. Macrophages exposed to acetylcholine - which is main parasympathetic neurotransmitter - are disarmed.
11. Impaired Cough
Afferent nerve endings richly innervate the pharynx, larynx, and airways to the level of the terminal bronchioles and extend into the lung parenchyma. They may also be located in the external auditory meatus (the auricular branch of the vagus nerve, or the Arnold nerve) and in the esophagus. Sensory signals travel via the vagus and superior laryngeal nerves to a region of the brainstem in the nucleus tractus solitarius vaguely identified as the “cough center.” The cough reflex involves a highly orchestrated series of involuntary muscular actions, with the potential for input from cortical pathways as well. The vocal cords adduct, leading to transient upper-airway occlusion. Expiratory muscles contract, generating posi- tive intrathoracic pressures as high as 300 mmHg. With sudden release of the laryngeal contraction, rapid expiratory flows are generated
Seizures
The first clinical use of vagus nerve stimulation was for refractory epilepsy. How exactly vagus nerve stimulation terminates seizures is not well understood, but some hypotheses have been developed. Here are three theories that attempt to explain why vagus nerve stimulation suppresses convulsions:
- Synchronization theory. Cervical vagus nerve stimulation induces EEG desynchronization. Desynchronization of overly synchronized neuronal activity may confer antiepileptic effects.
- Neurotransmitter theory. Krahl et al. found that lesioning hte locus ceruleus prevents the anticonvulsant effects of vagus nerve stimulation. Depleting norepinephrine in the brain also eliminates the anti-seizure effects of the vagus nerve stimulation. Finally, Ben-Menachem et al. observed increased GABA and decreased glutamate following vagus nerve stimulation.
- Cerebral blood flow theory. Henry showed that vagus nerve stimulation alters blood flow to numerous brain regions and may activate inhibitory structures in the brain. Excess vagus nerve activity induces fainting (syncope); this hypothesis is an extension of that observation.
References
-
http://healthland.time.com/2013/05/09/why-kindness-can-make-us-happier-healthier/?iid=hl-main-lead ↩
-
O'keane V, Dinan TG, Scott L, Corcoran C. Changes in hypothalamic-pituitary-adrenal axis measures after vagus nerve stimulation therapy in chronic depression. Biol Psychiatry. 2005;58(12):963-8. ↩
-
De ridder D, Kilgard M, Engineer N, Vanneste S. Placebo-controlled vagus nerve stimulation paired with tones in a patient with refractory tinnitus: a case report. Otol Neurotol. 2015;36(4):575-80. ↩
-
George MS, Ward HE, Ninan PT, et al. A pilot study of vagus nerve stimulation (VNS) for treatment-resistant anxiety disorders. Brain Stimul. 2008;1(2):112-21. ↩
-
Aydin MA, Salukhe TV, Wilke I, Willems S. Management and therapy of vasovagal syncope: A review. World J Cardiol. 2010;2(10):308-15. ↩
-
Richter WO, Geiss HC, Aleksic S, Schwandt P. Cardiac autonomic nerve function and insulin sensitivity in obese subjects. Int. J. Obes. Relat. Metab. Disord. 1996;20:966–969. ↩
-
Karason K, Molgaard H, Wikstrand J, Sjostrom L. Heart rate variability in obesity and the effect of weight loss. Am. J. Cardiol. 1999;83:1242–1247. ↩
-
Carnethon MR, Jacobs DR, Jr, Sidney S, Liu K. Influence of autonomic nervous system dysfunction on the development of type 2 diabetes: the CARDIA study. Diabetes Care. 2003;26:3035–3041. ↩
-
Gebhardt N, Bär KJ, Boettger MK, Grecksch G, Keilhoff G, Reichart R, et al. Vagus nerve stimulation ameliorated deficits in one-way active avoidance learning, and stimulated hippocampal neurogenesis in bulbectomized rats. Brain Stimul. 2012 In Press 42. ↩