Is Cannabis Linked To Depersonalization?
There's no question that Cannabis use can result in depersonalization.
Cannabis reliably and dose-dependently induces depersonalization symptoms, such as feeling detached from your body.
Depersonalization is the third most common mental health condition, after anxiety and depression. Yet it's rarely discussed or diagnosed by psychiatrists.
Cannabis has demonstrated therapeutic potential for various conditions. For example, it may treat seizures and chronic pain. Yet cannabis has been linked to depersonalization, psychosis, and other mental illnesses in vulnerable people.
This cannabis-mental illness link is understandably controversial in the medical community.
One lingering question is whether cannabis unmasks a latent tendency toward depersonalized states verses inducing depersonalization by itself. A gene x environment interaction seems much more likely. The medical literature seems to agree on two points:
- Cannabis use acutely can induce depersonalization
- However, genetics and stressful life events are more important causative factors in cannabis users who later develop persistent depersonalization
Many factors can contribute to depersonalization. But most cases are induced by either illicit drug use or severe stress.
Some interesting theories have been proposed about how cannabis can provoke depersonalization. THC (the active agent in cannabis) causes blood flow alterations that triggers a frontolimbic inhibitory mechanism. Researchers think this inhibitory mechanism might play a role in the depersonalizing effects of cannabis. More on this later!
What Does Depersonalization Feel Like?
If you were suffering from depersonalization, how would you know?
There are a few telltale signs:
- detachment from the body
- the sensation that there's a barrier (e.g., a pane of glass) separating you from reality
- an intense fear that you're going crazy
- visual distortions
- distorted perception of time
- numbed emotional response
Psychiatrists characterize depersonalization as a cluster of the following:
- anomalous body experience, including ‘somatosensory distortions’ or ‘perceptual alterations’, which encompass sensory distortions in various modalities
- emotional numbing
- anomalous subjective recall
- alienation from surroundings (i.e. derealization)
Here are some fun facts about depersonalization:
- Depersonalization is equally prevalant in men and women, but drug-induced depersonalization is more strongly associated with male gender and adolescence
- Depersonalization often co-occurs with other disorders (e.g., depression and anxiety)
- Because depersonalization is frequently co-morbid, even the most experienced psychiatrists overlook it. Despite being relatively common in the general population (1-2%), depersonalization is under-diagnosed.
- There's no cure for depersonalization and most medications have questionable efficacy for depersonalization8
Medications that affect serotonin, dopamine, and the opioid system have been tested as treatments for depersonalization. Results have generally been disappointing. But repetitive transcranial magnetic stimulation (rTMS) has demonstrated promising reductions of depersonalization symptoms in several case studies.9 These depersonalization treatments are discussed in greater detail here.
Evolution and Depersonalization
A tenant of evolution is that unfavorable traits are selected against and vanish from a population over time.
Researcher's have proposed that mental illness is a manifestation of exaggerated behaviors that can be adaptive in a more moderate form. Mild anxiety is clearly adaptive - it can protective you from harm's way.
Another example: mild depression in times of famine, for example, could be adaptive, because it decreases your motivation and metabolic rate.
In a similar vein, depersonalization may be an adaptation to extreme stress. Your brain is constantly "trying" to maintain homeostasis to return it its baseline state.
Intense stress might cause a reflex to kick in that suppresses emotional responses. But if this reflex overcorrects, it can leave you feeling numb and detached.
These ideas fit with observation that periods of depersonalization often follow anxiety attacks and traumatic events. For this reason, researchers believe the disorder acts as a protective mechanism to cope with stress.8
Causes of Depersonalization
One group1 of investigators asked whether the symptoms of depersonalization differed between drug-induced and stress-induced (chronic) depersonalization.
The authors enrolled nearly 400 participants and asked them a battery of questions. Next, they used the [Cambridge Depersonalization Scale (CDS)](https://www.ncbi.nlm.nih.gov/pubmed/10725532
) to evaluate survey responses.
You'll never guess what the most common illicit drug used by the participants was: cannabis. The runner up was ecstasy followed by other hallucinogens.
Surprisingly, the participants with chronic depersonalization demonstrated better improvement over time compared to the drug-induced group. I would expect the opposite. For example, the prognosis for amphetamine-induced psychosis is more favorable than psychosis related to schizophrenia.
Both drug-induced and chronic depersonalization groups responded similarly to to drugs and psychotherapy1.
Effects of Cannabis
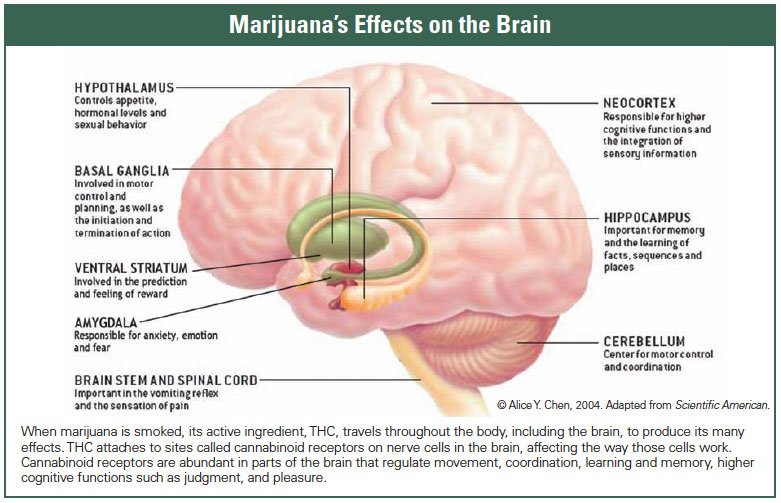
Cannabis binds cannabinoid receptors in the nervous system.
The activation of these receptors affects:
- pain regulation pathways
- motor activity
- mood
- higher cognitive processes
Cannabis' has demonstrated therapeutic potential as a treatment for pain, glaucoma, and seizures.
Used recreationally, cannabis elicits hunger, euphoria, relaxation, visual disturbances, alterations in perception, and depersonalization.2
Fortunately for us, researchers have directly investigated the cannabis-depersonalization link.
One of the earliest explorations of cannabis and depersonalization comes from Szymanski's paper3 published in 1981. Szymanski followed four different cases of cannabis users who experienced symptoms of depersonalization. All the patients started using marijuana after stressful events like the death of a close friend or the start of a new job.
The study sheds light on a few different issues:
- Chronic depersonalization symptoms matched how the study participants felt when acutely intoxication with cannabis
- The patients experienced emotional detachment and general sense of unreality
- Their symptoms persisted after discontinuing cannabis use. One possibility is that cannabis was continuing to influence their neurophysiology, since it can linger in the body for many weeks. Another possibility is that smoking cannabis precipitated a latent predisposition for depersonalization.
Szymanski emphasized the idea that depersonalization is an unconscious protective reflex against intense anxiety:
In all of these cases the patients considered their chronic symptoms to be identical to those experienced during acute intoxication. The patients tended to blame marijuanna for their distress, relegating psychosocial stressors to secondary importance. Even when their symptoms abated coincident with resolution or removal of the stressors, the patients did not appreciate their importance. This is consistent with psychodynamic theories of depersonalization that hold it to be an unconscious defense against intolerable anxiety.
Another more systematic paper, which drew on data from 35 studies, suggested that cannabis use increased the risk of developing psychosis.7 The cannabis-psychosis link is more well-documented than cannabis' association with psychosis.
The take-home message is that cannabis can adversely affect mental health in vulnerable people.
Role for Catechol-O-methyl transferase (COMT)?
Millions of people regularly consume cannabis with no obvious ill health effects. This begs the question: who's likely to experience adverse effects from cannabis?
One big determinant is genetics.
People with a polymorphism affecting the catechol-O-methyl transferase (COMT) gene might be more sensitive to the pyschotomimetic effects of cannabis.
The gene encodes the COMT enzyme which is vital for catecholamine degradation. Impaired dopamine metabolism is linked to the development of psychosis and schizophrenia. 2
A recent study examined cannabis-induced depersonalization in six adolescents. They note that depersonalization symptoms arise in adolescence at the same age when cannabis use peaks.
The first study participant was a man in his thirties who started smoking cannabis at 13 and at 17 started experiencing bouts of anxiety and a feeling of being in a dream. At age 20, he moved out of his parent's house and escalated his cannabis use and withdrew socially. When he realized that he had become socially phobic, he discontinued cannabis use. After discontinuation, he reported:
One day after cessation of cannabis use, he felt as if people around him were actors and wearing masks. While this experience soon vanished, he developed the chronic feeling of being in a dream, or of being surrounded by fog. He reported perceiving his environment in ‘2-D’ instead of ‘3-D’, and sometimes he felt as though he was ‘watching a movie’ and hearing himself speak from outside his own body.
The second patient smoked cannabis at age 15 and experienced intense anxiety.
Ever since he has felt like a stranger in his own world and his awareness of his own body is reduced. His movements feel ‘automatic’ and he feels outside his body. His voice often appears alien to him and familiar voices sound remote and unreal. Furthermore, he experiences recurrent ‘flashbacks’ with concomitant anxiety, and he persistently feels as if an invisible border exists between him and his environment, or as if he is looking at the world through inversed binoculars. He also reports frequent problems in dealing with incoming information from the outside. Subsequent to these symptoms he began feeling isolated and ‘trapped’ in a condition that nobody else knew about or noticed. None of the several doctors he consulted was able to explain his situation. He became worried about developing a severe and ‘terminal’ mental illness
The third study participant also started smoking cannabis at age 15 and reported the following:
He then developed anxiety and a ‘strange feeling in his mind’ that he was unable to better describe, and further developed an altered sense of time. It seemed as if things that he had recently done had taken place a long time ago. When writing on his computer, he saw his fingers still moving on the keyboard after he had already finished writing the text on the screen, as if the fingers were alien. Also, when he was playing the drums, he had the impression that the sound of the drums was long gone whilst he was still hitting the drums, or that the drums sounded remote. He often felt insecure about whether his environment was real or not. When he then stopped smoking cannabis, all these symptoms remitted and since then only reappear episodically when he feels emotional stress.
Five of the six patients reported anxiety following cannabis use. Heightened anxiety is linked to depersonalization. Of all emotional states, anxiety is the strongest predictor of depersonalization. All the patients believed the cannabis use was linked to their symptoms.4
The endocannabinoid system is responsible for regulating mood and pain pathways and responses to emotional stimuli. It also plays a role in modulating responses to stress.
A double-blind study demonstrated that cannabis can precipitate depersonalization in a dose-dependent manner. The effects of depersonalization were maximal 30 minutes after subjects smoked high-potency spliffs; subjects who smoked low-potency spliffs lacked these symptoms. Placebo smokers did not experience any depersonalization symptoms.5
The Frontolimbic Inhibitory Mechanism
Cannabis increases cerebral blood flow (CBF).
Researchers showed that the active ingredient in cannabis, tetrahydrocannabinol (THC), produced CBF changes and depersonalization symptoms. Fifty-nine patients were infused with a placebo, low-dose THC, or high-dose THC. CBF was monitored using positron emission tomography (PET).6
The groups that received both low and high doses of THC had an increase in CBF 30 minutes after infusion. CBF was largest in the anterior cingulate cortex (ACC) for both groups, but larger increases were noted in the right frontal cortex and right insula in the high-dose group. In addition, CBF decrease was noted in the basal ganglia, thalamus, amygdala, and hippocampus. The authors suggested the frontolimbic inhibitory mechanism and its resultant imbalance between frontal and limbic brain regions could serve as the neurological basis for depersonalization.6
Conversely, Stern's group argued that failure of frontolimbic inhibitory function plays a role in borderline personality disorder (BPD). BPD is characterized by mood instability and exaggerated emotional responses. In a sense, BPD is depersonalization's opposite.
The frontolimbic inhibitory mechanism may be a "neurological protective response" that plays a role in depersonalization. During high-anxiety states, the prefrontal cortex dampens the limbic system to better regulate emotions. As a result, people can detach from their emotional responses and become hyper-vigilant of their surroundings.4
That cannabis can precipitate depersonalization is well-established. How this happens also sheds light on the origin and mechanisms of depersonalization. Cannabis' effects on the frontolimbic inhibitory mechanism suggests a neurobiological origin for depersonalization.
References
-
Simeon D, Kozin DS, Segal K, Lerch B. [Is depersonalization disorder initiated by illicit drug use any different? A survey of 394 adults] (http://europepmc.org/abstract/med/19538903). J Clin Psychiatry. 2009;70(10):1358-64. ↩
-
Konopka LM. [Marijuana use: neuroscience perspective] (https://www.ncbi.nlm.nih.gov/pubmed/24891287). Croat Med J. 2014;55(3):281-3. ↩
-
Szymanski HV. [Prolonged depersonalization after marijuana use] (https://www.ncbi.nlm.nih.gov/pubmed/6969998). Am J Psychiatry. 1981;138(2):231-3. ↩
-
Hürlimann F, Kupferschmid S, Simon AE. [Cannabis-induced depersonalization disorder in adolescence] (https://www.ncbi.nlm.nih.gov/pubmed/22378193). Neuropsychobiology. 2012;65(3):141-6. ↩
-
Mathew RJ, Wilson WH, Humphreys D, Lowe JV, Weithe KE. [Depersonalization after marijuana smoking] (https://www.ncbi.nlm.nih.gov/pubmed/8490070). Biol Psychiatry. 1993;33(6):431-41. ↩
-
Mathew RJ, Wilson WH, Chiu NY, Turkington TG, Degrado TR, Coleman RE. [Regional cerebral blood flow and depersonalization after tetrahydrocannabinol administration] (https://www.ncbi.nlm.nih.gov/pubmed/10442442). Acta Psychiatr Scand. 1999;100(1):67-75. ↩
-
Moore THM, Zammit S, Lingford-Hughes A, Barnes TRE, Jones PB, Burke M, Lewis G. [Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review] (http://dx.doi.org/10.1016/S0140-6736(07)61162-3). The Lancet. 2007;370(9584):319-328. ↩
-
Sierra M. [Depersonalization disorder: pharmacological approaches] (https://www.ncbi.nlm.nih.gov/pubmed/18088198). Expert Rev Neurother. 2008;8(1):19-26. ↩
-
Jay EL, Nestler S, Sierra M, Mcclelland J, Kekic M, David AS. [Ventrolateral prefrontal cortex repetitive transcranial magnetic stimulation in the treatment of depersonalization disorder: A consecutive case series] (https://www.ncbi.nlm.nih.gov/pubmed/27104926). Psychiatry Res. 2016;240:118-22. ↩